Introduction
Understanding the financial landscape of Epic EMR is essential for healthcare organizations navigating the complexities of electronic medical records. With its expansive reach, managing over 64% of patient records globally, Epic EMR not only enhances patient care but also introduces significant financial implications through its diverse pricing models and implementation costs.
As organizations evaluate the initial investment against potential long-term benefits, a critical question emerges:
- How can healthcare providers ensure that their financial commitment to Epic EMR translates into tangible returns on investment and improved operational efficiency?
This inquiry is not just about cost; it’s about maximizing value in a rapidly evolving healthcare environment.
Explore the Basics of Epic EMR
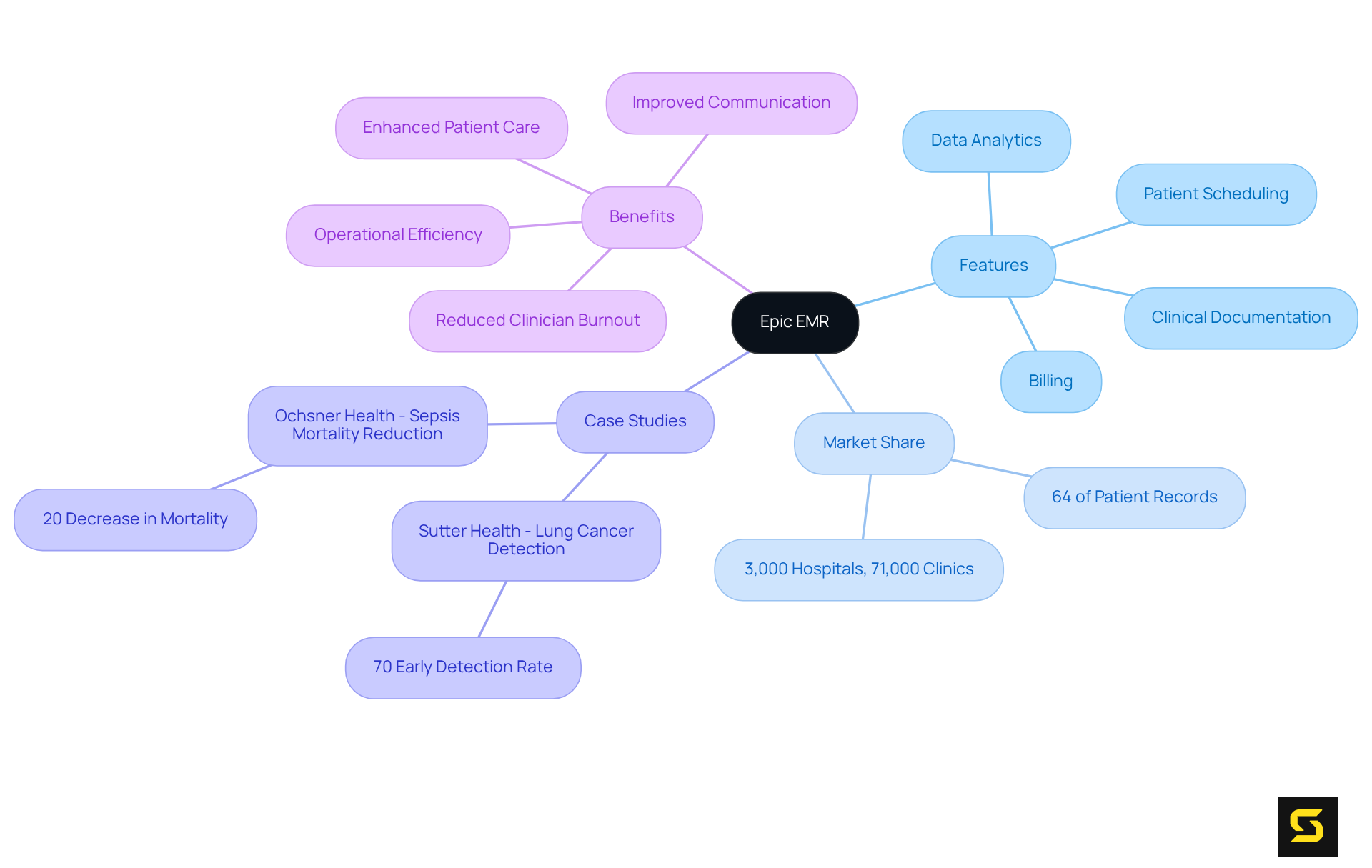
The EMR (Electronic Medical Record) is not just a software solution; it’s a transformative tool that significantly enhances patient care and operational efficiency in healthcare settings. By integrating essential features like patient scheduling, billing, clinical documentation, and data analytics into one cohesive platform, this EMR emerges as a leader in the electronic health record market, managing an impressive 64% of all patient records worldwide and utilized by over 3,000 hospitals and 71,000 clinics. Its intuitive user interface and robust capabilities foster improved communication among healthcare providers, a critical factor in delivering high-quality patient care.
Consider the case of Sutter Health, which has effectively harnessed a specific EHR and AI tools to boost early lung cancer detection, successfully identifying over 70% of cases at an early stage and thereby increasing survival rates. As Dr. Jason Wiesner aptly noted, the impact of early detection on treatment outcomes is profound. Furthermore, the company is actively developing AI tools aimed at reducing manual chart extraction, which not only enhances clinician efficiency but also alleviates burnout.
The MyChart patient portal is another vital component, playing a crucial role in enhancing patient engagement and communication. Understanding these fundamental elements is essential for evaluating the cost of epic emr, implementation strategies, and return on investment associated with the EMR system. Embrace the future of healthcare with an EMR that not only meets but exceeds expectations.
Analyze Epic EMR Pricing Models
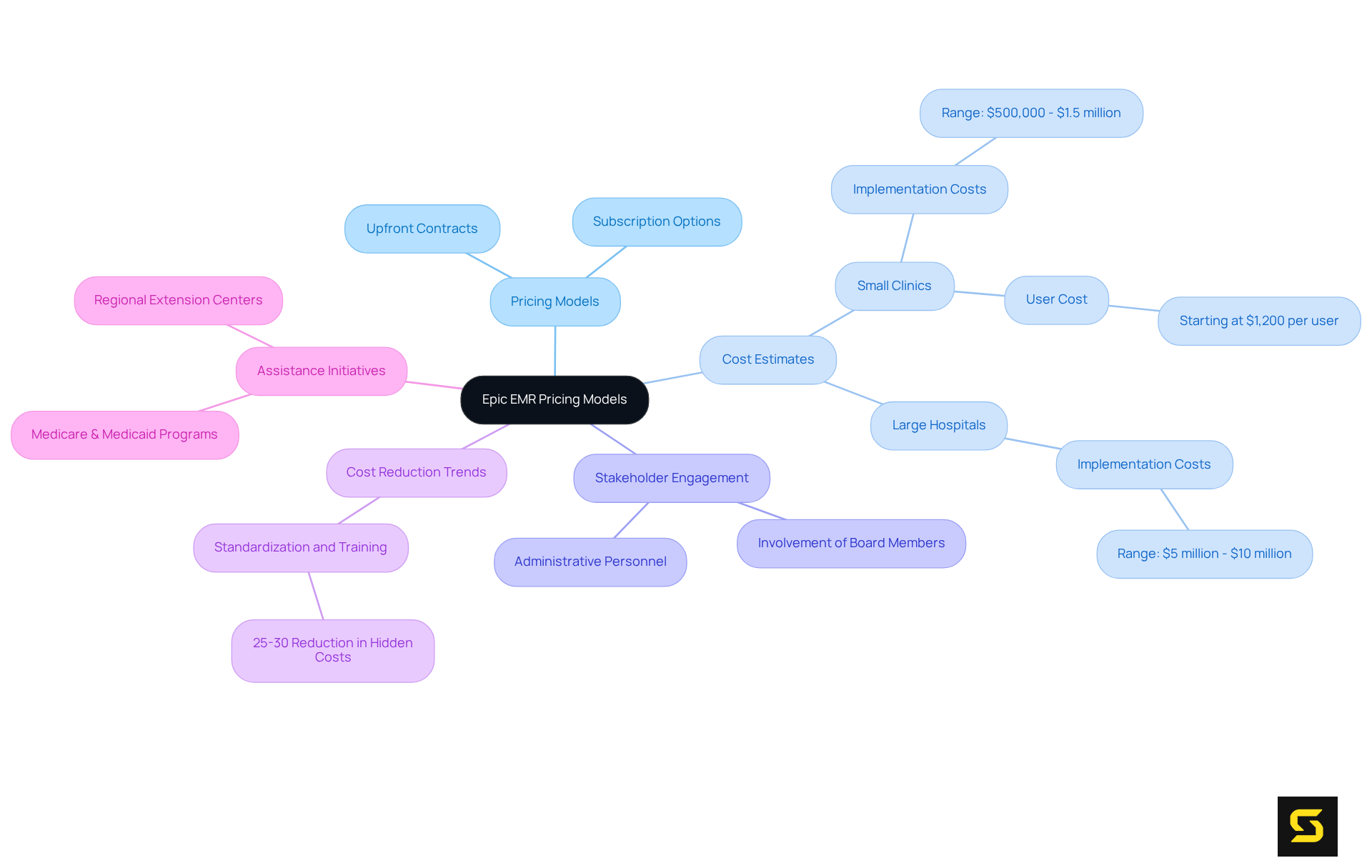
Epic EMR offers a range of pricing models that consider the cost of Epic EMR, including upfront contracts and subscription-based options, tailored to meet diverse organizational needs. For self-hosted solutions, the cost of Epic EMR typically starts at around $1,200 per user. The cost of Epic EMR implementation can vary significantly, with smaller clinics facing expenses between $500,000 and $1.5 million, while larger hospitals might encounter costs ranging from $5 million to $10 million.
Moreover, the cost of Epic EMR fluctuates based on user count and selected features, adding another layer of financial consideration. Engaging stakeholders - such as board members and administrative personnel - is crucial for addressing all expenses associated with the EMR system. A thorough understanding of the cost of Epic EMR and other pricing frameworks is essential for healthcare organizations, enabling them to evaluate their financial commitments effectively and align them with operational objectives.
Current trends indicate that organizations focusing on standardization and training can achieve a 25-30% reduction in hidden costs within the first two years post-implementation. This statistic underscores the importance of strategic financial planning in the integration of electronic medical record systems. Additionally, national assistance initiatives, like the Medicare & Medicaid Promoting Interoperability Programs, can alleviate the financial burden of adopting EHR systems, making it more feasible for organizations to implement this EMR.
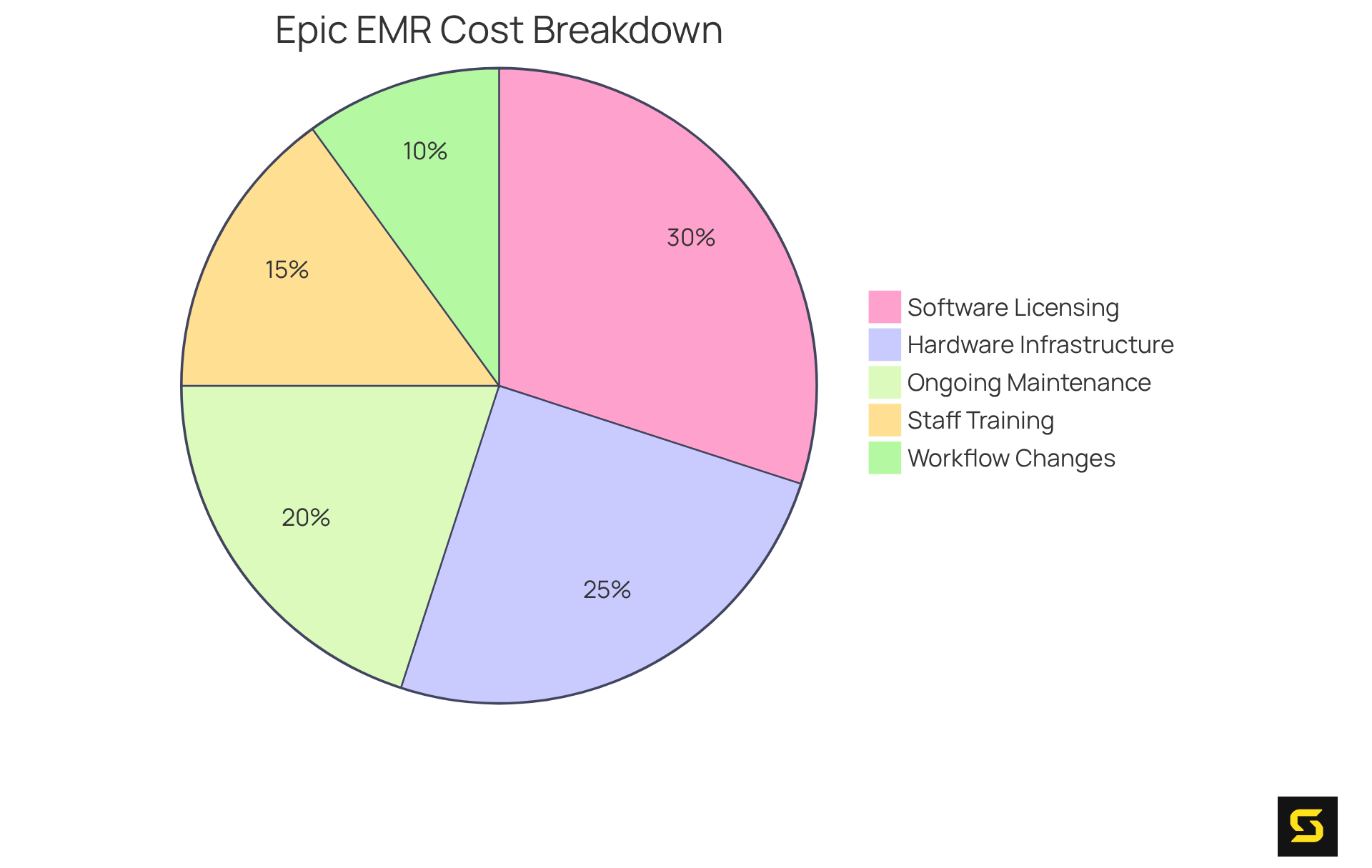
Evaluate Implementation Costs of Epic EMR
The cost of Epic EMR includes significant financial considerations such as software licensing, hardware infrastructure, and essential staff training. The cost of Epic EMR can vary widely in initial setup, with small practices potentially facing charges starting around $150,000, while larger hospital systems might incur expenses exceeding $10 million. Furthermore, the cost of Epic EMR includes ongoing maintenance and support that typically require 15-20% of the initial setup each year, translating to an additional $100,000 or more annually. This underscores the necessity for sustained investment in system upkeep.
Organizations must also account for expenses related to workflow changes and potential downtime during the transition. The risk of costly customizations arises if workflows are not optimized beforehand. A comprehensive assessment of the cost of Epic EMR, along with a benefit analysis and ROI projection, is crucial for healthcare providers to ensure successful implementation that aligns with their financial constraints and operational goals.
For instance, Lake Charles Memorial Health System dedicated 18 months to prepare for their MyChart EHR installation, highlighting the extensive planning required to manage expenses effectively. Moreover, healthcare leaders emphasize that investing in adequate training can mitigate implementation challenges. The average training cost is approximately $1,200 per end user, significantly impacting the overall return on investment.
By understanding these financial implications, organizations can navigate the complexities of EMR integration more effectively and enhance their return on investment.
Assess Long-Term Financial Implications and ROI
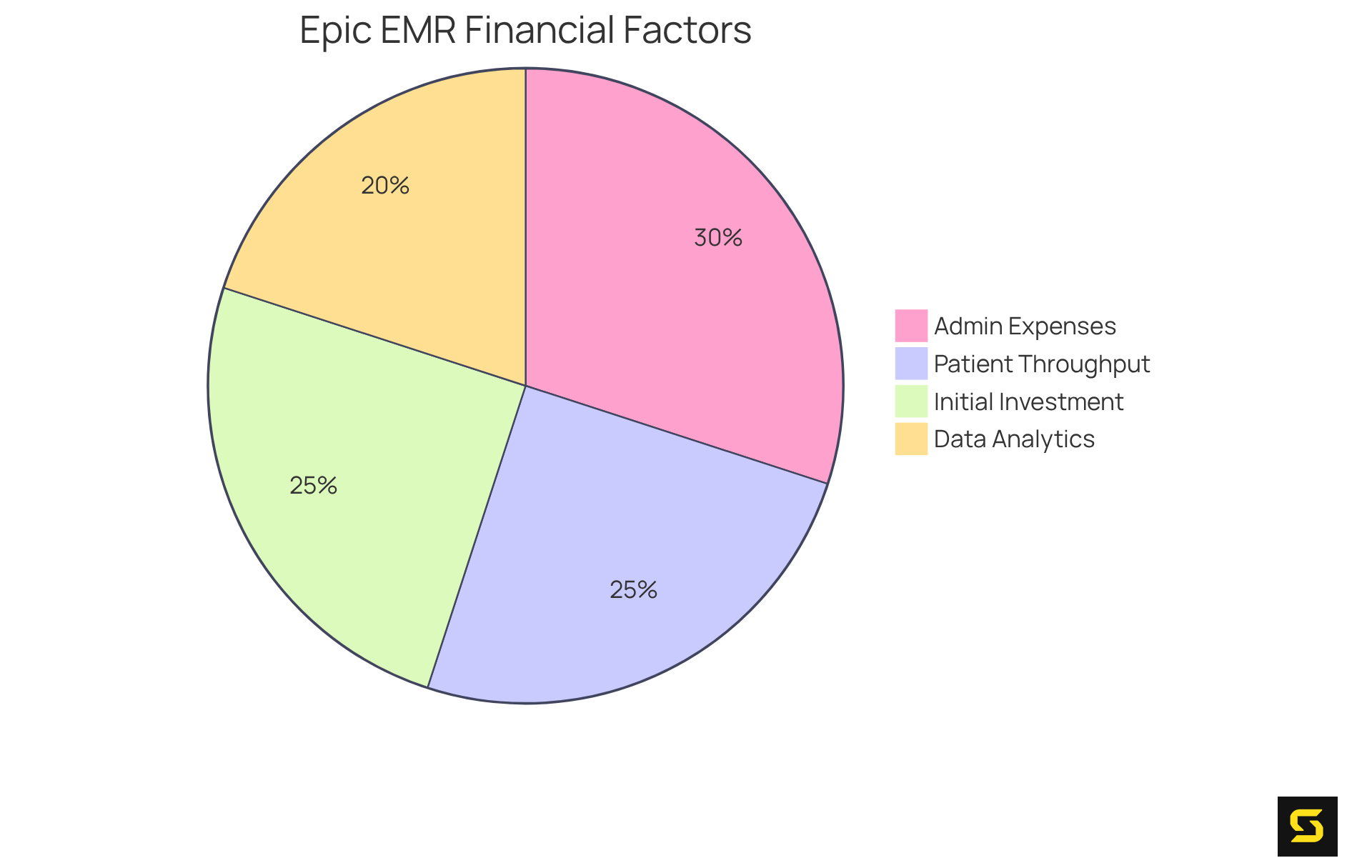
Assessing the long-term economic implications of the cost of Epic EMR requires a thorough examination of both direct and indirect expenses, as well as the anticipated benefits. While the initial investment can be substantial, healthcare organizations like NewYork-Presbyterian, with its innovative hospital-at-home program, have reported significant improvements in operational efficiency, reduced billing errors, and enhanced patient care. These factors collectively contribute to increased revenue over time.
For instance, organizations that refine their billing processes often see better cash flow and lower denial rates, leading to considerable financial gains within the first year post-implementation. A comprehensive ROI evaluation must consider:
- Decreased administrative expenses
- Improved patient throughput
- Enhanced data analytics capabilities
Moreover, ongoing enhancements and tailored training programs are essential for maximizing the system's potential and securing long-term economic benefits.
By juxtaposing these advantages against the cost of Epic EMR, which can exceed $500,000 for medium-sized organizations, healthcare entities can gain clearer insights into the viability of their investment. Furthermore, healthcare executives assert that the long-term financial benefits of EMR systems, when strategically implemented, can justify the initial costs through measurable improvements in patient outcomes and operational efficiencies.
In conclusion, the strategic implementation of Epic EMR not only promises enhanced operational capabilities but also positions healthcare organizations for sustainable financial success.
Conclusion
The integration of Epic EMR into healthcare organizations marks a crucial advancement in enhancing patient care and operational efficiency. This comprehensive electronic medical record system not only streamlines various healthcare processes but also promotes improved communication among providers, ultimately resulting in better patient outcomes. For healthcare leaders aiming to maximize their return on investment, understanding the associated costs - from initial implementation to long-term maintenance - is essential.
Throughout this article, we have explored key insights regarding the pricing models, implementation costs, and potential ROI of Epic EMR. While the upfront expenses can be significant, organizations that strategically plan and invest in training and optimization can reap substantial long-term benefits. Case studies from Sutter Health and NewYork-Presbyterian exemplify how effective utilization of Epic EMR can lead to enhanced operational efficiencies and improved patient care.
Given these findings, it is imperative for healthcare organizations to conduct thorough financial assessments and strategic planning when considering the adoption of Epic EMR. By embracing this transformative technology, healthcare providers can not only enhance their operational capabilities but also pave the way for sustainable financial success and improved patient outcomes in the future.
Frequently Asked Questions
What is Epic EMR?
Epic EMR (Electronic Medical Record) is a transformative tool designed to enhance patient care and operational efficiency in healthcare settings by integrating features like patient scheduling, billing, clinical documentation, and data analytics into one cohesive platform.
How widely is Epic EMR used?
Epic EMR manages 64% of all patient records worldwide and is utilized by over 3,000 hospitals and 71,000 clinics.
What are the benefits of using Epic EMR for healthcare providers?
Epic EMR fosters improved communication among healthcare providers, which is critical for delivering high-quality patient care, and its intuitive user interface enhances operational efficiency.
Can you provide an example of how Epic EMR has improved patient outcomes?
Sutter Health has effectively used Epic EMR and AI tools to boost early lung cancer detection, successfully identifying over 70% of cases at an early stage, which has increased survival rates.
What role does AI play in the use of Epic EMR?
Epic EMR is actively developing AI tools aimed at reducing manual chart extraction, enhancing clinician efficiency, and alleviating burnout among healthcare providers.
What is the MyChart patient portal?
The MyChart patient portal is a vital component of Epic EMR that enhances patient engagement and communication between patients and healthcare providers.
Why is it important to understand the fundamental elements of Epic EMR?
Understanding these elements is essential for evaluating the cost, implementation strategies, and return on investment associated with the Epic EMR system.





