Overview
This article delineates four essential steps that SaaS product owners must master for effective EHR implementation. It emphasizes the importance of:
- Establishing a clear roadmap
- Forming a dedicated implementation committee
- Developing a comprehensive training program
- Defining success factors alongside evaluation strategies
Each step is fortified by practical recommendations:
- Defining objectives to enhance patient care
- Engaging diverse stakeholders to ensure thorough oversight
- Utilizing key performance indicators to monitor the implementation's effectiveness
These strategies are crucial for ensuring a successful transition to electronic health records, paving the way for improved patient outcomes and operational efficiency.
Introduction
The landscape of healthcare technology is evolving rapidly, with Electronic Health Records (EHR) leading this transformation. For SaaS product owners, mastering the intricacies of EHR implementation is not merely a necessity; it is a strategic advantage that enhances patient care and streamlines operations. However, the path to successful EHR deployment is fraught with challenges. How can organizations ensure they navigate this complex process effectively? This guide outlines four essential steps that will empower product owners to create a robust implementation roadmap, engage stakeholders, and ultimately drive successful outcomes in their healthcare initiatives.
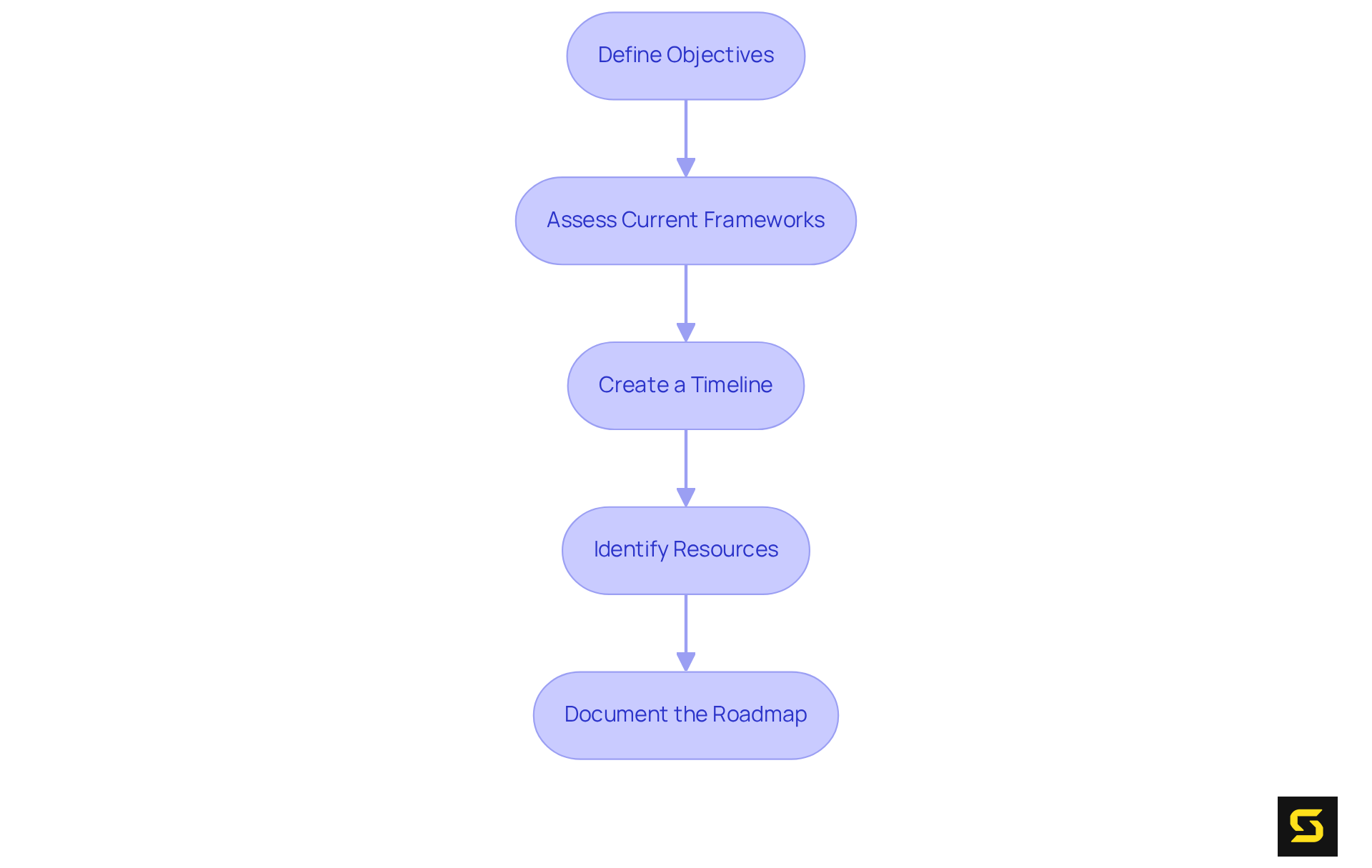
Establish Your EHR Implementation Roadmap
- Define Objectives: Begin by articulating the specific goals of your EHR deployment. What outcomes do you aim to achieve? This may encompass , improving data accessibility, or optimizing workflows. For example, EHRs have been shown to decrease medication errors by as much as 50% and reduce hospital readmissions by up to 20%, underscoring their capacity to significantly elevate patient safety and care quality. As Samantha McInnis, an expert in EHR implementation, asserts, "Defining clear objectives is crucial for aligning the implementation process with organizational goals."
- Assess Current Frameworks: Conduct a thorough evaluation of your existing frameworks and processes to pinpoint gaps and areas ripe for enhancement. This assessment will shape your strategic roadmap and assist in prioritizing essential features. Pay particular attention to interoperability, as effective communication between EHR systems is vital for achieving your objectives.
- Create a Timeline: Formulate a realistic timeline that encompasses all phases of execution, from initial planning to the go-live date. Segment the timeline into manageable phases, each with specific milestones. Incorporate regular audits and training into this timeline to ensure compliance with regulations and to proactively address any emerging challenges.
- Identify Resources: Ascertain the resources required for each phase, including personnel, technology, and budget considerations. It is imperative to have the right team in place to facilitate execution. Engaging physicians early in the process can significantly enhance adoption success and mitigate usability concerns.
- Document the Roadmap: Develop a visual representation of your roadmap, such as a Gantt chart or flowchart, to effectively communicate the plan to all stakeholders. This documentation will serve as a critical reference throughout the execution process, ensuring alignment and clarity among all parties involved.
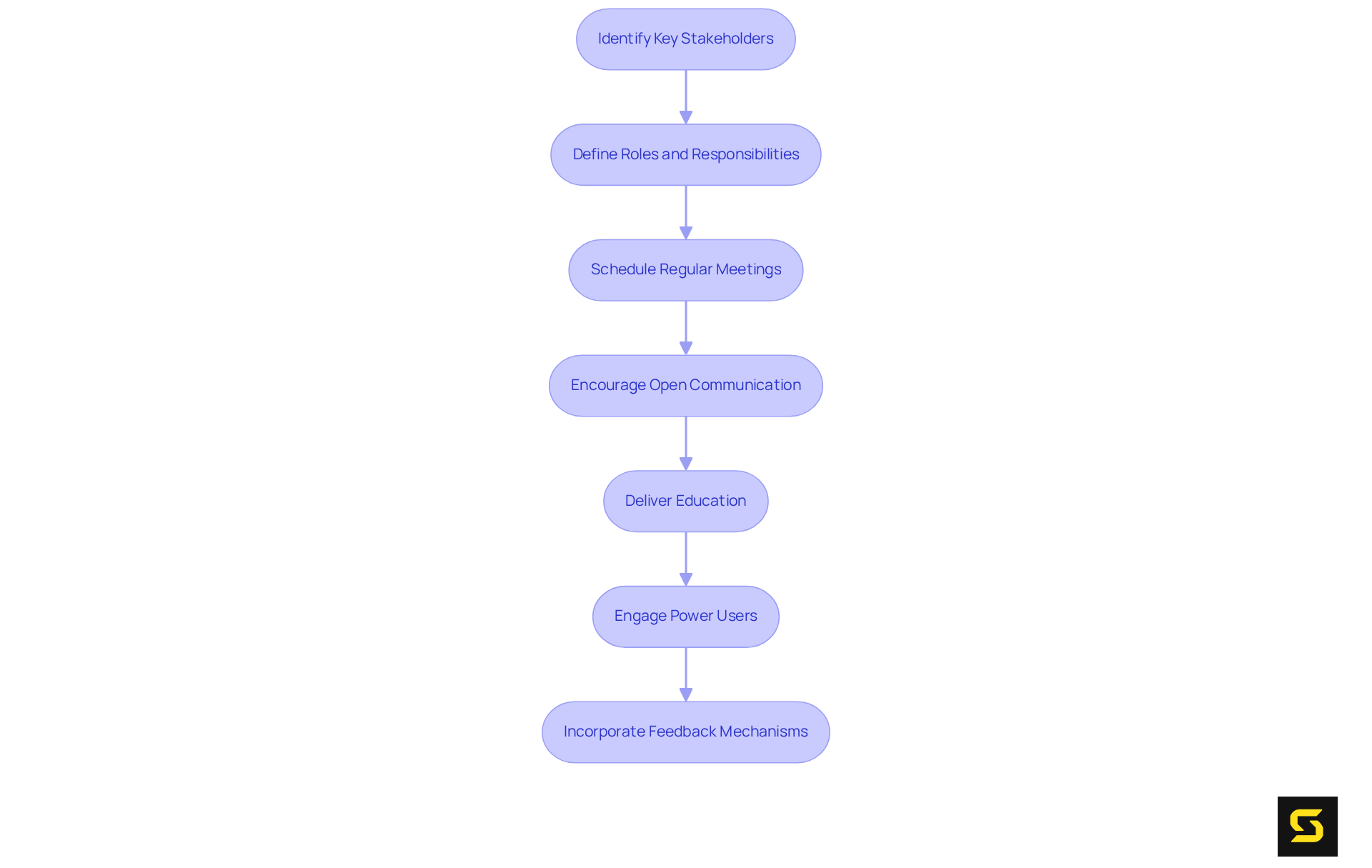
Form Your EHR Implementation Committee
- Identify Key Stakeholders: Establish a diverse advisory committee that encompasses representatives from clinical, administrative, and IT departments. This diversity ensures that all perspectives are considered, leading to a more comprehensive approach to EHR implementation.
- Define Roles and Responsibilities: Clearly outline the roles and responsibilities of each committee member. This clarity fosters accountability and streamlines decision-making processes, which are crucial for effective execution.
- Schedule Regular Meetings: Develop a consistent meeting schedule to assess progress, address challenges, and adjust the action plan as needed. Regular communication is essential for sustaining momentum and ensuring alignment among team members.
- Encourage Open Communication: Foster an environment that encourages open dialogue among committee members. Promoting the exchange of insights and concerns enhances problem-solving capabilities and cultivates innovation during the EHR implementation process.
- Deliver Education: Provide committee members with comprehensive training on EHR frameworks and implementation strategies. This preparation empowers them to make informed decisions and through EHR implementation.
- Engage Power Users: Identify and involve 'power users' who can facilitate peer-to-peer training and support. Their expertise can help others navigate the EHR platform more effectively, improving overall user satisfaction and reducing frustration.
- Incorporate Feedback Mechanisms: Establish feedback loops to gather input from all stakeholders throughout the implementation process. This practice not only enhances engagement but also ensures that the EHR implementation effectively addresses the needs of its users, ultimately leading to improved clinical outcomes.
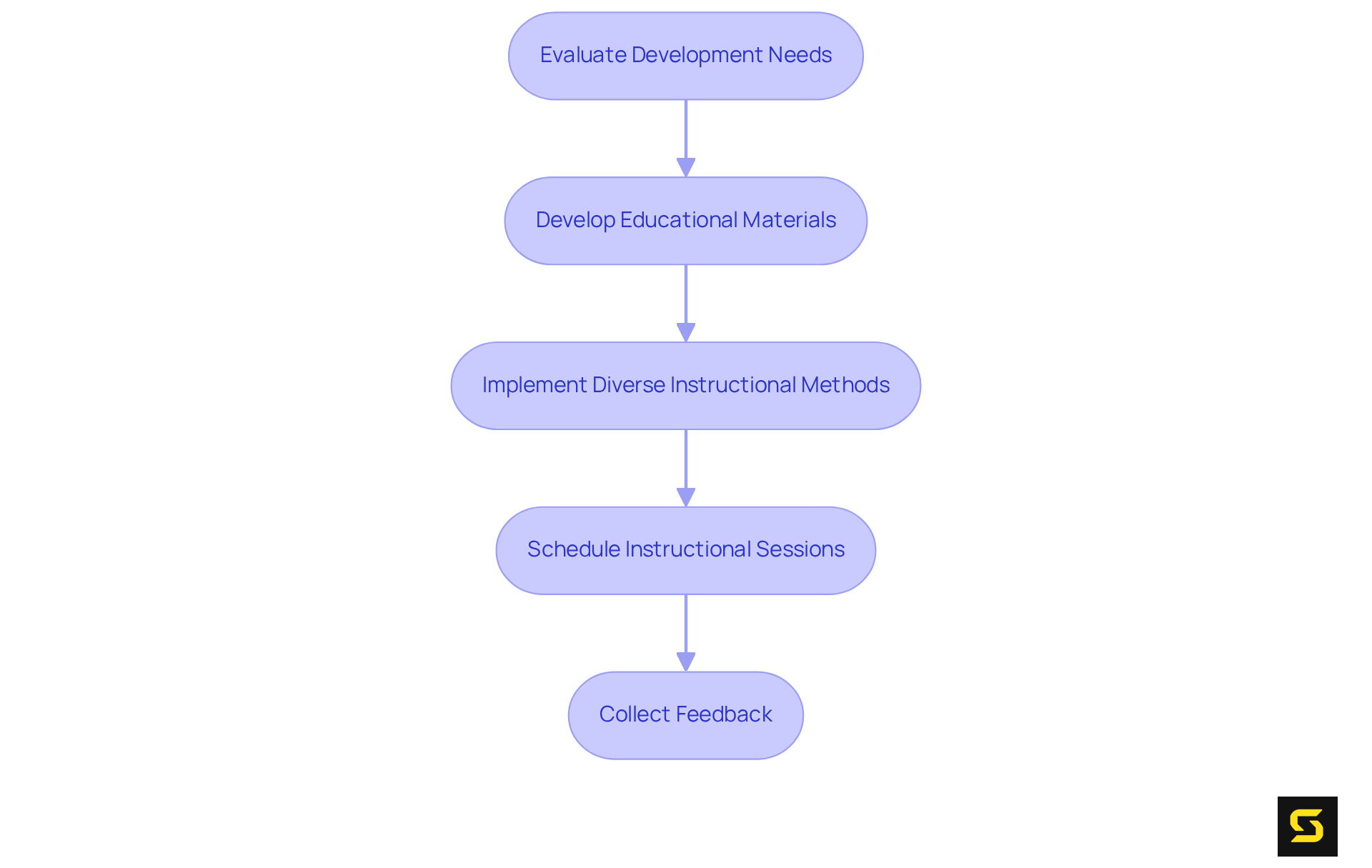
Develop a Comprehensive EHR Training Program
- Evaluate Development Needs: Begin with a thorough needs analysis to pinpoint the specific development requirements of diverse user groups. This evaluation must consider varying levels of technical proficiency, guaranteeing that every user receives the support they require.
- Develop Educational Materials: Assemble an extensive array of resources, including manuals, video tutorials, and quick reference guides. These materials should be easily accessible, enabling users to locate the information they need when necessary.
- Implement Diverse Instructional Methods: Employ a variety of instructional techniques to cater to different learning styles. This approach can encompass hands-on workshops, online courses, and personalized coaching sessions, all of which enhance engagement and retention. Additionally, integrating microlearning techniques can significantly boost knowledge retention by breaking down complex topics into digestible segments.
- Schedule Instructional Sessions: Plan instructional sessions well in advance of the go-live date. Providing multiple sessions ensures that all users have the chance to participate, thereby enhancing overall preparedness. Notably, organizations like M Health Fairview and UCHealth have successfully implemented centralized educational strategies that foster user involvement and satisfaction.
- Collect Feedback: Following each session, solicit input from participants to discern strengths and areas for improvement. This feedback loop is vital for refining future development initiatives and addressing ongoing challenges, ultimately resulting in heightened and resource utilization. Continuous training is essential as EHR platforms evolve, and inadequate training can lead to diminished efficiency and increased costs, underscoring the importance of a well-structured training program.
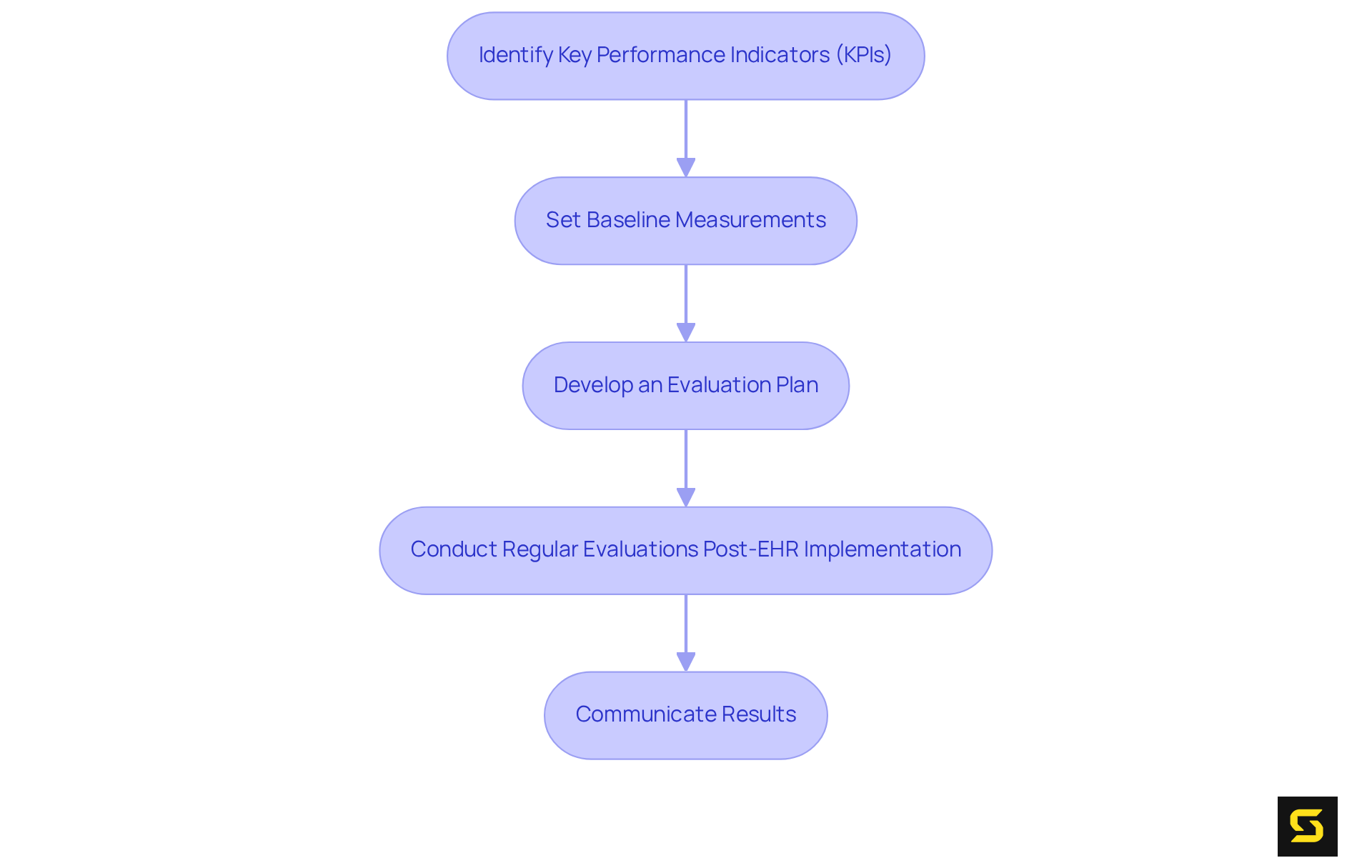
Define Success Factors and Evaluation Strategies
- Identify Key Performance Indicators (KPIs): Establish the essential KPIs for measuring the success of the EHR implementation. Common indicators include user satisfaction, operational uptime, and patient care enhancements. Monitoring patient satisfaction is crucial, as it directly relates to the prompt and precise information provided by the EHR platform, underscoring its significance in enhancing patient experiences.
- Set Baseline Measurements: Prior to execution, it is vital to create baseline measurements for each KPI. This foundational data serves as a benchmark for assessing the impact of the new framework. Collecting retrospective information on clinical, operational, and financial metrics from 1-2 years prior to execution can provide a historical baseline for comparison.
- Develop an Evaluation Plan: Formulate a comprehensive evaluation plan outlining how and when each KPI will be measured. This plan should include both qualitative and quantitative assessments, ensuring a holistic view of the EHR's performance. Integrating third-party analytics can significantly enhance data analysis capabilities, providing advanced reporting and predictive insights that are essential for informed decision-making.
- Conduct Regular Evaluations Post-EHR Implementation: Schedule consistent evaluations to measure progress against the defined KPIs. Regular are critical for reliable decision-making, ensuring that the information captured in EHRs is correct and consistent. These evaluations should pinpoint areas for enhancement and inform necessary modifications to optimize performance. Recognizing challenges such as data inconsistencies and resistance to change is also essential for a balanced evaluation process.
- Communicate Results: Share evaluation results with all stakeholders to illustrate the impact of the EHR implementation. Clear and consistent communication is a critical success factor, fostering trust and encouraging ongoing support for the system. As Wim Niewold emphasizes, motivating colleagues for new practices is essential. Engaging staff early while highlighting the supportive role of data can help mitigate resistance to change, ensuring a smoother transition and integration.
Conclusion
The successful implementation of an Electronic Health Record (EHR) system is paramount for healthcare organizations that aspire to elevate patient care and optimize operations. This endeavor hinges on meticulous planning, effective communication, and continuous engagement with all stakeholders involved. By adhering to best practices, healthcare organizations can not only achieve their implementation goals but also enhance the overall quality of patient care. Embracing these strategies will pave the way for a more efficient and effective healthcare delivery system, ultimately benefiting both providers and patients alike.
Frequently Asked Questions
What is the first step in establishing an EHR implementation roadmap?
The first step is to define specific objectives for the EHR deployment, such as enhancing patient care, improving data accessibility, or optimizing workflows.
Why is it important to define clear objectives for EHR implementation?
Defining clear objectives is crucial for aligning the implementation process with organizational goals and can lead to significant improvements in patient safety and care quality.
How should organizations assess their current frameworks before EHR implementation?
Organizations should conduct a thorough evaluation of existing frameworks and processes to identify gaps and areas for enhancement, focusing particularly on interoperability.
What should be included in the timeline for EHR implementation?
The timeline should encompass all phases of execution, from initial planning to the go-live date, and should include specific milestones, regular audits, and training.
What resources need to be identified for EHR implementation?
Resources required include personnel, technology, and budget considerations. Engaging physicians early can enhance adoption success and address usability concerns.
How can organizations document their EHR implementation roadmap?
Organizations can create a visual representation of the roadmap, such as a Gantt chart or flowchart, to communicate the plan effectively to all stakeholders.





